Sitting in class one day I was confused why I could no longer see the writing on the board. It was not a matter of needing glasses, it looked as if there was a flashing hole in the middle of my vision (later to be known as an aura). Then came the head pain, I would not even classify it as a headache because it was magnified much more than typical headache pain. After this, things started to get weird. I would lose feeling in my fingers and toes, be unable to speak or have slurred speech, and experienced dizziness resulting in emesis or unconsciousness. I began to see a neurologist and my symptoms resulted in a diagnosis of basilar migraines, an extraordinarily rare form of migraine originating in the brainstem. Part of what deems this migraine so rare is its high prevalence in women, specifically young women, with a mean age of onset at 20.3 ± 11.7 years (Guomin Ying et al., 2014, Kadian R et al., 2023). Migraines overall, regardless of subtype, encompass a higher prevalence in women than in men. Explanations and mechanisms for this will be further analyzed here.
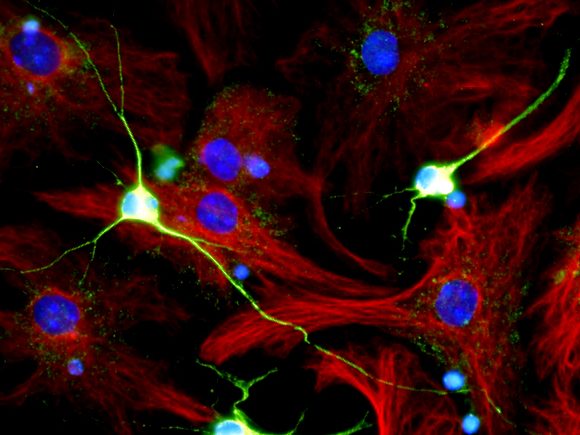
Everyone has distinctive variations of migraines, but systematically, the start of them commences with the overactivation of the hypothalamus and brainstem areas before symptom onset. Specifically, the hypothalamus is a point of connection and regulation to many nerves and cortical structures with the focus of keeping the body at homeostasis. After this overactivation, the aura phase occurs which is described as a “visual disturbance” due to the overactivation of retinal ganglion cells and increased temporary depression in the cortex (King, 2024). From here, an interesting dichotomy occurs because the brain cannot feel pain yet there are intense pain-like sensations in the brain associated with migraines. The pain sensation is due to blood vessels dilating near the meningeal brain layers, irritating the trigeminal cranial nerve and other surrounding pain-sensing (nociceptive) areas not in the brain. The brain itself does not contain these nociceptors, while its neighboring structures do. Nonetheless, after the pain or “attack” phase, there are persistent symptoms that can be anywhere up to two days after such as trouble concentrating or sensitivity to light (Charles A, et al., 2017).
What is an element that differs greatly between the neurobiology of men and women? Hormones. Thus, these are a viable measure to look at why women experience migraines far more often than men. The prevalence of migraines in women is highest in the segment between the onset of puberty and the start of menopause, times when hormone production is highest. It is common for migraines to cease once a woman enters menopause, further evidence that hormones play a critical role in migraine management. Even a woman’s menstrual cycle influences migraine prevalence, where frequent migraines occur before or during menstruation and additionally ovulation (Chaudhary A. et al., 2021). Many hormones fluctuate during a woman’s cycle, one of the key players in this is estrogen. Estrogen is thought to be the main hormone accounting for the occurrence of migraines, it also has significantly lower levels in men. Studies were accomplished that proved hormonal birth control improved migraine prevalence in young women due to its ability to better regulate estrogen levels, but there also were cases where it worked in the other direction and caused migraines in those who had not suffered from them previously. Other hormones such as progesterone or luteinizing hormone may also have an effect depending on the patient and could be an interesting further field of study.
Genetics may also be a cause for migraines, yet it is still a fairly unknown field. In this case, it appears the environment may have a stronger impact than genetics since migraines are regularly brought on by triggers in someone’s environment. It could be argued the genetics of someone’s hormones is what makes them susceptible to migraines or not. I have not faced a migraine since I was eighteen, prime evidence of migraines being attributed to the hormone fluctuations of puberty, as seen especially in basilar migraines. The fact that the brain cannot feel pain but still feels as if one’s brain is in pain only scratches the surface of the complexity of migraines, making them more than just a headache.
References
Charles A, Brennan KC. The neurobiology of migraine. Handb Clin Neurol. 2017;97:99-108. doi: 10.1016/S0072-9752(10)97007-3. PMID: 20816413; PMCID: PMC5494713.
Chaudhary A. Migraine Associated with Menstruation An Overlooked Trigger. JNMA J Nepal Med Assoc. 2021 Jul 1;59(238):611-613. doi: 10.31729/jnma.6332. PMID: 34508410; PMCID: PMC8369556.
Guomin Ying, Wen Fan, Nan Li, Jing Wang, Wangwen Li, Ge Tan, Jiying Zhou, Clinical Characteristics of Basilar-Type Migraine in the Neurological Clinic of a University Hospital, Pain Medicine, Volume 15, Issue 7, July 2014, Pages 1230–1235, https://doi.org/10.1111/pme.12402
Kadian R, Shankar Kikkeri N, Kumar A. Basilar Migraine. [Updated 2023 Jun 26]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK507878/
King, Gwendalyn. “Migraine.” NES 464. 25 Feb. 2024, Omaha, Creighton University.