Among lysosomal storage disorders, few are as relentlessly progressive or as poorly understood as neuronopathic Gaucher disease (nGD). This rare, autosomal inherited lipid storage disorder results from recessive mutations in the GBA1 gene, which encodes β-glucocerebrosidase (Gcase), a lysosomal enzyme. Deficiency of this enzyme results in the accumulation of glucosylceramide and a secondary loss of related glycosphingolipids (gangliosides) not being broken down. The buildup of harmful fatty materials in the cells has severe effects on neuronal function and leads to progressive damage to the CNS as seen in type 2 and type 3 Gaucher disease. Those with type 2 die before two years of age from rapid neurodegeneration, while those with chronic type 3 have more slowly progressing neurological symptoms including seizures, oculomotor disturbances, and cognitive decline (Arévalo et al., 2022). Although enzyme replacement and substrate reduction therapies may aid in treating systemic forms of nGD, “there is no effective treatment for severe brain damage that may affect people with Gaucher Types 2 and 3 disease” (NINDS, 2025). Enzyme replacement therapy does not cross the blood-brain barrier (Collin-Histed et al., 2023), making treatment of nGD more challenging.
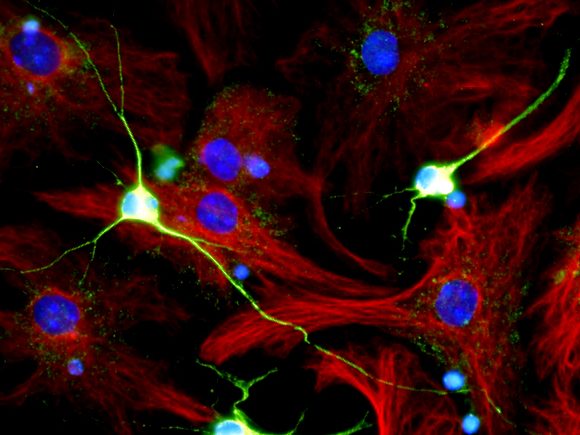
Mechanistically, recent research shows that nGD pathology extends beyond a lysosomal storage issue. The loss of Gcase enzyme activity disrupts interactions of cellular organelles (lysosomes, endoplasmic reticulum, mitochondria) as seen in altered calcium regulation, decreased mitochondrial metabolism, and lipid signaling changes (Arévalo et al., 2022). Mitochondrial dysfunction is an early symptom of nGD, with reduced ATP production and increased reactive oxygen species resulting in neuronal stress and death. Microglial activation also plays a major role, as studies in animal models and patient plasma demonstrate that Gba rescue in microglia/macrophage compartments can extend survival, “which was further enhanced upon treatment with brain-permeant inhibitor of glucosylceramide synthase” (Boddupalli et al., 2022, p. 5). A neuroinflammatory environment with elevated cytokines contributes to neurodegeneration. These findings reveal that nGD involves a more complex cascade beyond a singular lysosomal defect. In addition, accumulation of lipids and α-synuclein interferes with synaptic vesicle recycling and neuronal connectivity, linking molecular pathology to the motor and cognitive symptoms seen in clinical settings (Ginns et al., 2014).
Further evidence looks at the dysregulation of cellular growth pathways in the cells contributing to disease progression. Messelodi et al. (2023) demonstrated that glucocerebrosidase deficiency activates the Hippo signaling cascade, which suppresses cell proliferation and promotes neuronal death. In both Drosophila models and human induced pluripotent stem cell-derived neurons, loss of glucocerebrosidase function leads to activation of the Hippo signaling pathway, resulting in reduced cell growth and neuronal vulnerability (Messelodi et al., 2023). “Hippo signaling has been established in neuroinflammation, neuronal cell differentiation, and neuronal death, where its role in mechano-transduction and regulation of cell growth are catching more and more attention” (Messelodi et al., 2023). Restoring enzyme activity of Gcase and inhibiting Hippo signaling pathway may lead to restored mitochondrial health and neuronal appearance. This poses the Hippo pathway as a potential therapeutic target alongside lysosomal repair therapy.
Treating such a rare yet severe disease without centralized data proves challenging. The Global Neuronopathic Gaucher Disease Registry (GARDIAN) compiles data from over twenty countries (approximately 400 patients with nGD), showing how the L444P mutation is the most prevalent and that phenotypic severity varies widely (Collin-Histed et al., 2023). There is a clear need for a standardized neurological scoring system and biomarkers that monitor disease progression to account for the wide variation among patients. Even those with identical GBA1 genotypes had different expressions, pointing to the influence of environmental factors and potential modifying genes. Recent advancements in small-molecule chaperones and gene-therapy approaches offer more hope that brain-penetrating treatments may correct the enzyme deficiency in nGD (Migdalska-Richards & Schapira, 2016).
Neuronopathic Gaucher disease shows how a single enzymatic deficiency can cascade into cellular dysfunction in multiple organelles and result in widespread neurodegeneration. The resistance to current treatments furthers the clinical severity of Type 2 and 3 nGD, often resulting in managing complications of Gaucher disease rather than the disease itself. Major gaps remain in understanding the molecular cascade that links lysosomal dysfunction to inflammation, Hippo pathway dysregulation, and neuronal loss. Continued research further exploring the causal sequence of events is crucial for developing therapies that can have an impact across the blood-brain barrier offering patients and families hope for an effective treatment.
References
Arévalo, N. B., Lamaizon, C. M., Cavieres, V. A., Burgos, P. V., Álvarez, A. R., Yañez, M. J., & Zanlungo, S. (2022). Neuronopathic Gaucher disease: Beyond lysosomal dysfunction. Frontiers in Molecular Neuroscience, 15, 934820. https://doi.org/10.3389/fnmol.2022.934820
Boddupalli, C. S., Nair, S., McGowan, J. R., Platt, F. M., & Mistry, P. K. (2022). Neuroinflammation in neuronopathic Gaucher disease: Role of microglia and NK cells, biomarkers, and response to substrate reduction therapy. eLife, 11, e79830. https://doi.org/10.7554/eLife.79830
Collin-Histed, T., Stoodley, M., Beusterien, K., Elstein, D., Jaffe, D. H., Revel-Vilk, S., & Davies, E. H., on behalf of the International Gaucher Alliance. (2023). A global neuronopathic Gaucher disease registry (GARDIAN): A patient-led initiative. Orphanet Journal of Rare Diseases, 18, 195. https://doi.org/10.1186/s13023-023-02828-w
Ginns, E. I., Mak, S.-K., Ko, N., Karlgren, J., Akbarian, S., Chou, V. P., Lim, J., Erickson, R. P., & Sulzer, D. (2014). Neuroinflammation and α-synuclein accumulation in response to glucocerebrosidase deficiency are accompanied by synaptic dysfunction. Molecular Genetics and Metabolism, 111(2), 152–162. https://doi.org/10.1016/j.ymgme.2013.12.003
Messelodi, D., Strocchi, S., Bertuccio, S. N., et al. (2023). Neuronopathic Gaucher disease models reveal defects in cell growth promoted by Hippo pathway activation. Communications Biology, 6, 431. https://doi.org/10.1038/s42003-023-04813-2
Migdalska-Richards, A., & Schapira, A. H. V. (2016). The relationship between glucocerebrosidase mutations and Parkinson disease. Journal of Neurochemistry, 139(S1), 77–90. https://onlinelibrary.wiley.com/doi/10.1111/jnc.13385
National Institute of Neurological Disorders and Stroke (NINDS). (2025, March 7). Lipid storage diseases. National Institutes of Health. https://www.ninds.nih.gov/health-information/disorders/lipid-storage-diseases