Complex Regional Pain Syndrome (CRPS) remains one of the most perplexing and clinically challenging pain disorders known to scientists. Despite an abundance of research, a single cause has yet to be determined, and researchers have yet to pinpoint an exact mechanism behind its action. In the meantime, CRPS patients endure prolonged intense pain, functional impairment, and a substantial financial burden for health care. Recent advances in neuroimaging, immunology, and neuromodulation are uncovering the multifaceted interactions between peripheral inflammation, autonomic dysfunction, and central sensitization, providing the means for new treatments to solve the question of how and why does CRPS develop?
CRPS is a chronic pain condition, often developed in response to physical trauma or surgery. Affecting roughly 0.03-0.07% of the population of the U.S. with about 200,000 cases reported each year, CRPS can be classified as Type I or II, with Type I occurring after illness/injury and Type II being associated with specific nerve damage (Briggi, D. R., et al; National Institute of Neurological Disorders and Stroke (n.d.)). The most prominent symptom of CRPS includes allodynia and hyperalgesia pain in the affected limb(s). However, CRPS can be accompanied by a wide variety of symptoms, such as changes in skin texture, temperature, and color, swelling of the affected limb, sweating, nail, hair, and bone growth, stiffness in affected joints, bone thinning, impaired muscle strength, and movement disorders. CRPS disproportionately affects more women than men, with roughly 72.5% of patients being female.
Pathophysiologically, CRPS is the result of immune-mediated inflammation, autonomic nervous system dysfunction, and/or degeneration of small (c and Aδ) nerve fibers (Briggi, D. R., et al). CRPS affects neurotransmitter levels of the central nervous system contributing to vasomotor dysfunction, a common symptom in which the affected limb is reported to be warmer than the healthy limb early on in CRPS, while later on its colder (Goebel, A., & Barker, C.). However, about 20% of CRPS cases report that the affected limb was perpetually colder than the healthy limb. This shift in relative temperature suggests that activity in vasoconstrictor neurons changes over time, with norepinephrine levels in the venous effluent above the affected limb being lower. This data suggests that thermoregulatory impairment is caused by functional changes triggered by the initial physical trauma to the brainstem, spinal cord, or brain. Not only does CRPS cause an increase in hormonal responses, but an increase in inflammatory responses is seen as well.
Additionally, levels of TNFα and interleukine 6 (IL-6) are greater on the affected limb of CRPS patients than the healthy one and are higher in CRPS patients than fracture patients who do not ultimately develop CRPS. Levels of soluble TNF receptors and the pro-inflammatory cytokines TNF, IL-1 and IL-8 are increased, and anti-inflammatory cytokines such as IL-4, IL-10, and TGFβ1 are decreased in early CRPS (Goebel, A., & Barker, C.). These changes in cytokine levels provide a strong correlation to the mechanical hyperalgesia, swelling, and skin irritation seen in patients.
Recent studies have additionally suggested the role of the immune system in patients with longstanding CRPS, such as a higher percentage of the pro-inflammatory CD14+CD16+ monocytes/macrophage subgroup, lower plasma levels of the anti-inflammatory cytokine IL-10, and increased IL-1β and IL-6 cytokine levels in spinal fluid from chronic CRPS patients (Goebel, A., & Barker, C.).
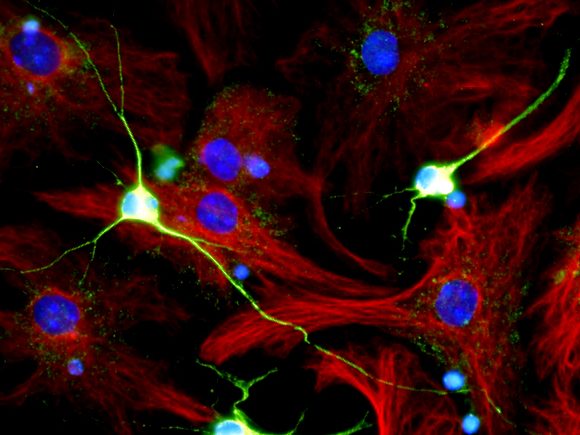
Undergoing functional and structural changes in the central nervous system, central sensitization leads to increased excitability of neurons in the spinal cord. This directly mirrors the changes that take place in emotional aspects of pain–in areas such as the amygdala, anterior cingulate gyrus, and prefrontal cortex (Goebel, A., & Barker, C.). One key component of central sensitization is the activation/up-regulation of glutamate receptors (such as NMDA receptors), enhancing signal transmission in the nociceptive circuitry from the spinal cord to the cortex. That is, neurons become more responsive to pain signals, even in the absence of stimuli. Thus, central sensitization can cause chronic pain, hyperalgesia, and allodynia (Goebel, A., & Barker, C.).
One potential treatment option is the intravenous infusion of the NMDA receptor antagonist: ketamine. Over several days, patients are injected with ketamine, which often results in significant pain reduction for up to 11 weeks in CRPS patients. This long-lasting analgesic effect suggests that ketamine imparts long-term desensitization of the NMDA receptors and other NMDA-mediated processes. However, not all CRPS symptoms, such as dystonia–a movement disorder causing contractions–respond to ketamine infusions, and not all CRPS patients receive relief via ketamine infusions either (Goebel, A., & Barker, C.).
In summary, CRPS stands at a crossroads, as despite significant progress in clarifying its complexity, breakthroughs in its treatments remain elusive. This evolving picture now implicates a dynamic interplay among peripheral changes in immune responses, maladaptive sensory plasticity, and dysfunctional autonomic pathways. The interaction between mechanistic insight and clinical translation will require collaborative, multidisciplinary efforts, additional studies, and more refined experimental models. Only by combining molecular, physiological, and clinical threads can neuroscientists move toward interventions that are truly disease-modifying in CRPS. Works Cited
Briggi, D. R., Reilly, J., Garcia, J., & Kupperman, W. (2025). SCS for CRPS: A Review of Cost-Effectiveness Models. Current Pain and Headache Reports, 29, 75. https://doi.org/10.1007/s11916-025-01388-x (SpringerLink)
National Institute of Neurological Disorders and Stroke. (n.d.). Complex Regional Pain Syndrome. U.S. Department of Health & Human Services. Retrieved from https://www.ninds.nih.gov/health-information/disorders/complex-regional-pain-syndrome
Goebel, A., & Barker, C. (2017). Complex regional pain syndrome in adults: UK guidelines for diagnosis, referral and management in primary and secondary care. Practical Pain Management. (Note: based on the PMC article you linked, the full reference would need verification.) Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5511749/